How much do you know about the aftermath of a nonfatal opioid overdose? Take our 10-question quiz to find out.
How much do you know about the aftermath of a nonfatal opioid overdose? Take our 10-question quiz to find out.

How much do you know about fibromyalgia? Take our 12-question quiz to find out your fibromyalgia IQ.

What new drugs should you know about from the second quarter of 2018? Scroll through our quick slideshow to find out.

Do you do locum tenens work or think you might be interested? Our app reviewer looks at 5 apps that help you plan, stay organized, manage budgets, and relax.
Patient Care scoured the web to find the top news in medicine this month that could affect your practice. Which ones made the cut?
The gap in Medicare Part D coverage, aka "the donut hole," may be a problem for many of your older patients, starting right about now.
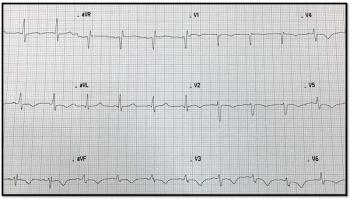
Are this young woman’s chest pain and SOB a reaction to Levaquin, started a few days ago? She’s had a similar reaction to other antibiotics. Your Dx?
How can you avoid at least these 5 key reasons for a call? One pharmacist has some guidance.
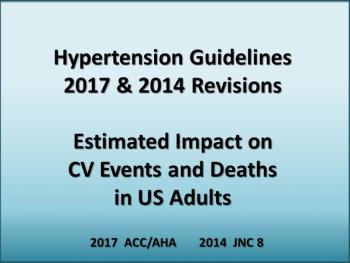
What impact could the latest 2017 hypertension guidelines have on your patients? Click through our quick slideshow to find out.

Money talks in a new study showing financial incentives, in addition to free smoking cessation aids, help employees quit smoking at a higher rate.

Our app reviewer picked out the top 5 apps in geriatric care. Scroll through our quick slideshow to get the highlights.

At-a-glance: Research on opioid addiction, exergaming for Alzheimer patients, medical cannabis for chronic pain, and more.
Risk of non-severe statin muscle pain was reduced in T2DM patients taking both metformin and statins, according to this recent study.

Who gets the cardioprotective agents? Are newer agents affordable? And, how low should A1c go?

Talking to your patients about cost of care can be difficult, but these five strategies are sure to help.

Test your literature scanning skills with our short, 5-question quiz on different asthma interventions in school-aged children.
Naloxone should be available to all at risk for opioid overdose and their caregivers, says the US Surgeon General.
How would you manage a patient with dementia and agitation? Take our 4-question case challenge from the 2018 ACP Internal Medicine Meeting to find out.

Get updated on the newest fibromyalgia research from the 2018 ACP Internal Medicine Meeting, the basis of this 5-question quiz.
Our app reviewer picked the top 5 apps that every primary care physician should have to stay up-to-date with current medical news. Check out our slideshow to find out more.