
They breathe in more air than do normal-weight persons, exposing them to more air pollutants and making them more vulnerable to asthma and other pulmonary diseases.

They breathe in more air than do normal-weight persons, exposing them to more air pollutants and making them more vulnerable to asthma and other pulmonary diseases.
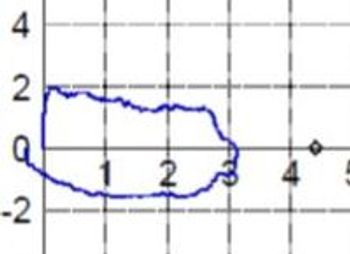
The patient presents 6 weeks after a prolonged hospitalization for pancreatitis. More details and the office spirometry tracing here.

In the news: respiratory disease underdiagnosed, Alzheimer biomarkers, Crohn disease microbiome, migraine device, sleep apnea and diabetes.


A simple way to prevent asthma or treat wheezing may be to eat flaxseed or take some kind of probiotic.

Several related health concerns-including asthma, pericarditis, and pneumonia-are treatable within the primary care office.

Re-expansion pulmonary edema is noncardiogenic and follows re-expansion of the lung after thoracentesis is performed for large amounts of pleural effusion or for pneumothorax.
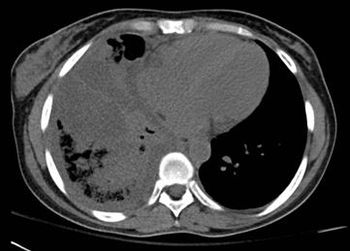
A young woman experienced acute onset of high fever, productive cough, and right-sided pleuritic pain. She was not in sickle cell crisis. Do the images here shed light on cause of symptoms?

A link was found between low vitamin A levels and the incidence of diarrhea with vomiting and cough with fever.

Obesity/respiratory infections; lung disease/cognitive function; Q&A/alcohol dependence. Why are these pairs linked? Get 3 answers plus 2 more questions in this week’s quiz, here.

Persons who are obese are at increased risk for catching the flu and other potentially serious respiratory diseases.

Obstructive lung disease may be linked with problems with memory and information processing. The more diminished the airflow, the greater the impairment.

The first confirmed case in North America this year has led the CDC to issue a health advisory reminding physicians about the symptoms and treatment.

Primary care physicians treat the majority of patients with respiratory diseases, where diagnosis often depends on early recognition of suggestive symptoms. This week’s photo quiz offers several presentations to test your knowledge.
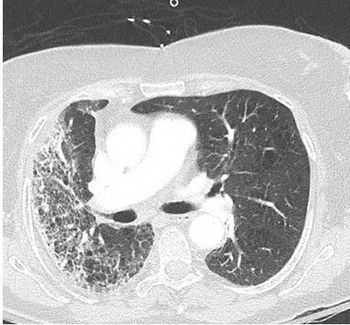
Results of a physical examination and CT scan of the chest offer clues to this patient's diagnosis.


A PET/CT scan shows uptake of tracer consistent with malignancy in the left lower lobe and mediastinal nodes. What would be your next step?

For patients with asthma or COPD, PL554 has the potential to both reverse bronchodilation and reduce inflammation more quickly and with fewer adverse effects.

This is an opportunity for primary care to help avert a public health catastrophe. Physicians need to take ownership over this issue and demand more time for URI patients-E&M criteria do not capture what is lost when these visits are viewed simply as “Level 2 Office Visit, CPT 99212.”

This case focuses on duplicate therapy resulting from the use of prescription medications, which can result in serious adverse effects.

Influenza infection may contribute to increases in cardiovascular hospitalizations and elevated rates of acute myocardial infarction (MI).

Respiratory symptoms are a major reason why outpatients seek medical care, and primary care physicians who treat children frequently see pneumonia. This week’s photo essay tests your knowledge of respiratory problems in kids.

Simple weight reduction may improve the management of asthma in obese patients, according to a new study

Vaccination against influenza substantially reduces the disease’s burden in the United States each year, according to the results of a unique look at the impact of vaccinations.

A unique cell phone application that targets minority adolescents who have asthma aims to reduce exacerbations of the condition and emergency department visits.