
Arunabh Talwar, MD
Articles by Arunabh Talwar, MD



A 62-year-old woman was seen prior to cholecystectomy. She had no cardiac or pulmonary disorders. Examination was unremarkable other than a purplish-reddish, lace-like pattern on the thighs and forearms.

A 26-year-old man presented with sudden onset of palpitations and shortness of breath after incidentally taking tadalafil. He had no other symptoms and no history of illnesses during childhood. He drank socially but denied smoking and use of illicit drugs.


A 61-year-old man with arthritis and an 80-pack-year smoking history presented with fever, dyspnea, and productive cough of a week’s duration that did not respond to outpatient treatment with levofloxacin.

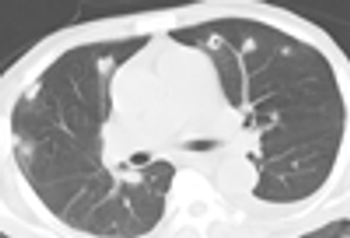
A 47-year-old man with HIV infection presented with progressive dyspnea and worsening productive cough for the past 3 weeks. He also reported increasingly purulent sputum production. The patient reported being adherent to his antiretroviral regimen, and he had an admission CD4+ cell count of 550/μL. He did not have any previous opportunistic infections, and he denied any drug or tobacco use, recent travel, and ill contacts.

A 71-year-old man who had received a diagnosis of emphysema 12 years ago was referred by his primary care physician to the pulmonary clinic. His symptoms were well controlled until a few months ago, when he complained of mild shortness of breath on physical activity. However, the shortness of breath worsened and became a significant limiting factor. He also had a persistent dry cough.

ABSTRACT: The most common causes of chylothorax are neoplasm-particularly lymphoma-and trauma. The usual presentingsymptom is dyspnea resulting from the accumulationof pleural fluid. The diagnosis of chylothorax is established bymeasuring triglyceride levels in the pleural fluid; a triglyceridelevel of greater than 110 mg/dL supports the diagnosis. The initialapproach to management involves chest tube drainage ofthe pleural space. The administration of medium-chain triglyceridesas a source of fat is often useful. If drainage remains unchanged,parenteral alimentation should be started. Surgicalintervention is indicated if conservative management is notsuccessful or if nutritional deterioration is imminent. If chylothoraxpersists after ligation of the thoracic duct, options mayinclude percutaneous embolization, pleuroperitoneal shunt,and pleurodesis. (J Respir Dis. 2008;29(8):325-333)

A 39-year-old woman presented with dry cough, which she had had for 3 months. She had mild intermittent asthma and a 5 pack-year smoking history. Her symptoms started after an upper respiratory tract infection and persisted despite multiple courses of antibiotics, decongestants, and corticosteroids.

A 5-month-old boy presented with fever, cough, and tachypnea that he had had for 1 month. There also was a history of poor weight gain for 2 months. The child was born full-term at a private hospital, and the mother's antenatal course was uneventful. There was no postnatal history of bleeding, jaundice, diarrhea, poor feeding, vomiting, or seizures. There was no family history of tuberculosis.

abstract: Tuberculous pericarditis, while relatively rare in the United States, is an important cause of pericardial disease in countries where tuberculosis is prevalent. Patients are most likely to present with chronic disease--effusive and/or constrictive. Those with effusive pericarditis often present with tamponade. Patients with constrictive pericarditis exhibit features of systemic and pulmonary venous congestion. An elevated level of adenosine deaminase in pericardial fluid is a good marker for tuberculosis. The presence of granulomas or case-ation necrosis in pericardial tissue confirms the diagnosis. If treatment of effusive tuberculous pericarditis is delayed, constrictive or effusive-constrictive disease usually develops, resulting in a high mortality risk. In addition to a standard antituberculosis regimen, treatment of tuberculous pericarditis may include adjuvant therapy with corticosteroids, pericardiocentesis, and/or pericardiectomy. (J Respir Dis. 2007;28(7):278-282)

The patient was a 41-year-old manwith a history of HIV infection diagnosed10 years before admission.He had been noncompliant withtreatment, and therapy with tenofovir,efavirenz, and lamivudinehad not been started until 2 monthsbefore admission, when he presentedto another hospital. At thetime, his CD4+ cell count was156/µL and his viral load was45,743 copies/mL. He also had ahistory of incarceration; had usedinjection drugs, cocaine, alcohol,and marijuana; and had a 20-packyeartobacco history.

A 66-year-old man presented with weight loss for 2 months, loss of appetite for several weeks, and abnormal chest radiographic findings. He denied chest pain, cough, fever, chills, shortness of breath, and chest trauma. He was an active smoker, with a 50-pack-year history of smok- ing, and a cocaine and alcohol abuser. His history included treatment of hypertension for 10 years and treatment of pulmonary tuberculosis 14 years previously.

Endobronchial foreign bodies can be life-threatening, but once they are detected, they can usually be removed, leading to prompt resolution of symptoms. Chest radiography and CT scanning can be helpful in some cases, but bronchoscopy is necessary for definitive diagnosis and treatment.

Abstract: Spinal tuberculosis is the most common form of osteoarticular involvement in patients with tuberculosis. Localized pain is a common presenting symptom. In patients who do not present until vertebral wedging and collapse have occurred, a localized knuckle kyphosis is obvious, especially in the dorsal spine. In some patients, a retropharyngeal abscess develops, causing dysphagia, dyspnea, and/or hoarseness. Peripheral joint tuberculosis is characterized by an insidious onset of slowly progressive, painful, and swollen monoarthropathy, most commonly affecting the hip or knee. The radiologic features include juxta-articular osteoporosis, peripheral osseous erosion, and gradual narrowing of the interosseous space. Treatment involves antituberculosis drugs; the indications for surgery are relatively limited. (J Respir Dis. 2005; 26(12):543-546)

Abstract: In addition to causing pulmonary disease, infection with Mycobacterium tuberculosis can result in a wide range of extrapulmonary manifestations, including abdominal involvement. Patients with acute tuberculous peritonitis typically present with fever, weight loss, night sweats, and abdominal pain and swelling. Intestinal tuberculosis is characterized by weight loss, anorexia, and abdominal pain (usually in the right lower quadrant). A palpable abdominal mass may be present. Patients with primary hepatic tuberculosis may have a hard, nodular liver or recurrent jaundice. The workup may involve tuberculin skin testing, imaging studies, fine-needle aspiration, colonoscopy, and peritoneal biopsy. Percutaneous liver biopsy and laparoscopy are the main methods of diagnosing primary hepatic tuberculosis. Treatment includes antituberculosis drug therapy and, in some cases, surgery. (J Respir Dis. 2005;26(11):485-488)

Abstract: Tuberculous meningitis has several different clinical presentations, including an acute meningitic syndrome simulating pyogenic meningitis, status epilepticus, stroke syndrome, and movement disorders. Cranial nerve palsies and seizures occur in about one third of patients, and vision loss is reported by almost 50%. The cerebrospinal fluid (CSF) typically shows moderately elevated levels of lymphocytes and protein and low levels of glucose. The demonstration of acid-fast bacilli in the CSF smear or Mycobacterium tuberculosis in culture confirms the diagnosis. CNS tuberculosis may also manifest as intracranial tuberculomas. The characteristic CT and MRI finding is a nodular enhancing lesion with a central hypointensity. Antituberculosis treatment should be initiated promptly when either tuberculous meningitis or tuberculoma is suspected. (J Respir Dis. 2005;26(9):392-400)

Abstract: Pleural tuberculosis and lymph node involvement are the most common extrapulmonary manifestations of tuberculosis. Most patients with pleural involvement complain of pleuritic chest pain, nonproductive cough, and dyspnea. The pleural effusion is usually unilateral and small to moderate in size. The diagnosis depends on the demonstration of acid-fast bacilli in pleural fluid or biopsy specimens, or the presence of caseous granulomas in the pleura. The gold standard for the diagnosis of lymph node tuberculosis is the identification of mycobacteria in smears on fine-needle aspiration cytopathology, histopathology, or mycobacterial culture. On ultrasonography and CT, the lymph nodes show enlargement with hypoechoic/hypodense areas that demonstrate central necrosis and peripheral rim enhancement or calcification. Treatment involves the combination of 4 antituberculosis drugs for 2 months, followed by 2-drug therapy for 4 months. (J Respir Dis. 2005;26(8):326-332)
Latest Updated Articles
 Bronchoscopy Clinic: Emerging options for managing foreign-body aspiration
Bronchoscopy Clinic: Emerging options for managing foreign-body aspirationPublished: February 1st 2006 | Updated:
 Extrapulmonary tuberculosis, part 2: CNS involvement
Extrapulmonary tuberculosis, part 2: CNS involvementPublished: September 1st 2005 | Updated:
 Extrapulmonary tuberculosis, part 4: Skeletal involvement
Extrapulmonary tuberculosis, part 4: Skeletal involvementPublished: December 1st 2005 | Updated:
 Diagnostic Puzzlers: What caused this patient's chest wall mass?
Diagnostic Puzzlers: What caused this patient's chest wall mass?Published: April 1st 2006 | Updated:
 Case In Point: Coexisting Hodgkin disease and lung cancer in a patient with AIDS
Case In Point: Coexisting Hodgkin disease and lung cancer in a patient with AIDSPublished: May 1st 2006 | Updated:
