
I was “foggy” on when and how to apply screens for lung cancer with low-dose CT, but a perfect model for a 3-question template provided answers.

I was “foggy” on when and how to apply screens for lung cancer with low-dose CT, but a perfect model for a 3-question template provided answers.
This slideshow highlights facts and figures about the number 1 diagnostic category in primary care.
Three studies culled from the very recent literature offer insights into prevention and treatment of pneumonia in adults. Highlights in this slide show.
What brings patients to your office-and not the specialty office down the street? Insights in this slideshow.
The 13-valent pneumococcal conjugate vaccine reduced nearly by half vaccine-type community acquired pneumonia in adults aged 65 years and older.
Risk of MI, stroke, and fatal coronary heart disease remained elevated among some patients hospitalized for pneumonia up to 10 years after the index event.

Food choices and dietary supplements may impact progression and management of respiratory disease. Try 6 quick questions on the topic and find out what you know.
Asthma and the metabolic syndrome may be more closely related than once believed. A short slide show summarizes key studies of known connections.

COPD challenges, asthma in children, smoking deaths-highlights of recent research findings in these key areas of respiratory disease.
What do you get when you cross asthma with COPD? How does an asthma Dx reduce antibiotic Rx? And what about vitamin D and asthma, anyway? Get answers and evidence in 5 easy pages.

Aspirin-exacerbated respiratory disease (AERD) is chronic, often severe asthma. Episodes can be life-threatening. Find out what you know about AERD after answering these 6 short questions.
Making a good match between a young patient and an inhaler device is a first step toward optimal asthma management. Find a brief review of how to make that match in this short slide show.

Is there a connection between this patient’s symptoms and the thin red-brown lines under his nails? Answer this question and 4 others in this quiz.

The risk of new-onset obstructive sleep apnea appears to be greater in persons who have asthma. Treating one may help the other.

Long-acting beta-agonists offer benefits in COPD. Not true for inhaled corticosteroids for most, it turns out.
What flu vaccine should you recommend this year for children over age 2? A look at the data . . .

Drugs, diseases, guidelines, databases-all at the touch of an app. Here: a selection of smartphone/tablet applications that may make your clinical practice a little easier this coming year.

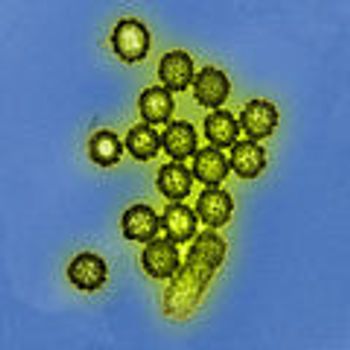
The enterovirus story continues to evolve: here are 6 things clinicians need to know now.
When you want to distinguish between asbestosis and silicosis, what imaging finding is inconsistent with the former disease?

Nail clubbing may occur with many conditions. In these two patients, it heralded lung cancer.
Drug-induced hypersensitivity pneumonitis, drug-induced organizing pneumonia, radiation-induced lung injury, allergic fungal rhinosinusitis, pulmonary tuberculosis, empyema-this week’s slide show sheds light on several presentations.

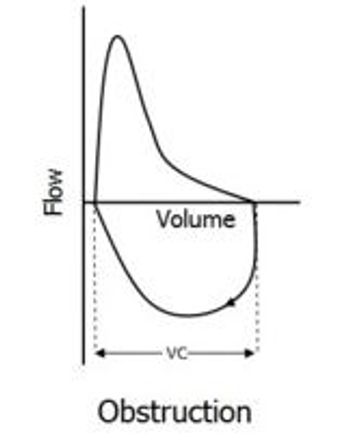
Pulmonary edema, tracheal stenosis, pulmonary embolism, pulmonary sarcoidosis, respiratory bronchiolitis interstitial lung disease, giant bullous emphysema-a close look at a variety of troublesome lung conditions.
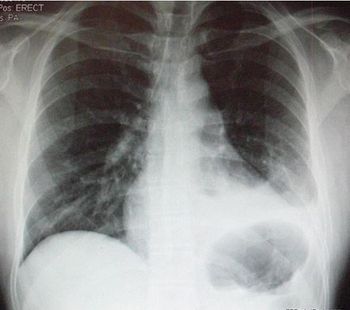
Recovery from a hemopneumothorax had progressed well for this 29-year-old man until today when he presents to the ED with dyspnea and pleuritic chest pain. What do you see on the chest x-ray?

Persistent symptoms of hemothorax or pneumothorax, in the absence of new x-ray findings require further inquiry, including chest CT, to rule out PE.

A new study shows that the risk of chronic obstructive pulmonary disease increases with obesity. Yet, the risk was increased in underweight persons as well.