
After suffering with a severe, disabling headache for 2 weeks, a 20-year-old soldier sought medical treatment. He had no significant medical history other than his 6-year history of smoking.

After suffering with a severe, disabling headache for 2 weeks, a 20-year-old soldier sought medical treatment. He had no significant medical history other than his 6-year history of smoking.

After more than 15 years of wondering what the “white specks” on his legs were, a 64-year-old man consulted his physician. The patient was taking medication to control hypertension; he was otherwise healthy.
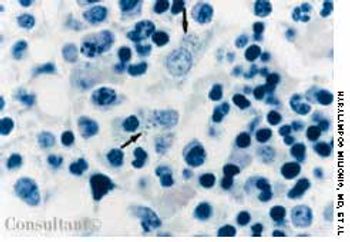
Fever occurring twice daily, accompanied by profuse sweating, anorexia, and malaise of 15 days' duration resulted in hospitalization of a 31-year-old woman. At this time, her temperature was 37.6°C (99.7°F); blood pressure, 110/70 mm Hg; pulse rate, 90 beats per minute; and respiratory rate, 18 breaths per minute. A palpable spleen was about 3 to 5 cm below the left subcostal margin. Neither lymphadenopathy nor hepatomegaly was noted.

A 65-year-old woman, who was confined to a wheelchair because of severe rheumatoid arthritis, was concerned about nodules that had erupted on her fingers and hands during the previous 3 weeks. Her medical history included colon cancer, chronic renal insufficiency, anemia, and hypertension. The nonpruritic nodules were painful when they began to form under the skin; however, once they erupted, the pain disappeared.

A 68-year-old man presented to the emergency department (ED) complaining of an itchy rash over his body. His past medical history included hypertension, contact dermatitis, and penicillin allergy.

A 45-year-old man complained of blood in his urine. The patient had a 7-year history of chronic renal failure secondary to hypertension; he had undergone hemodialysis for the past 5 years.
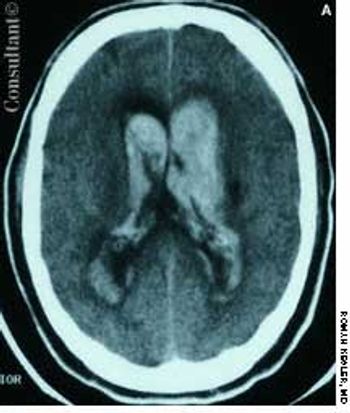
A 57-year-old man complained of a severe headache of sudden onset while he was lifting heavy boxes. Within minutes, he collapsed and became unconscious. On arrival at the emergency department, the patient was deeply comatose. His pupils were 7 mm, fixed, and unreactive to light; brainstem reflexes were absent, and he was unresponsive to noxious stimulation. His blood pressure was 210/120 mm Hg; he had no known history of hypertension.
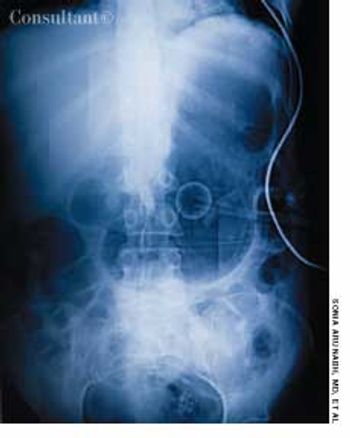
A 70-year-old man was brought from a nursing home to the emergency department with abdominal distention and vomiting of recent onset and a 2-day history of fever and abdominal pain. The patient had chronic obstructive pulmonary disease, type 2 diabetes mellitus, and hypertension. His gastric feeding tube, which had been placed via percutaneous endoscopic gastrostomy, was blocked.
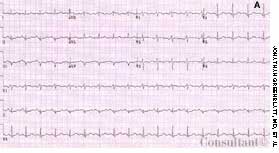
A 67-year-old woman presented to the emergency department (ED) with severe, sharp, central chest pain of sudden onset and mild shortness of breath. The pain had been present for 15 minutes. The patient was obese; her medical history included hypertension, myocardial infarction, and osteoarthritis.

More than 25% of hypertensive patients have white-coat hypertension, which has also been called "office hypertension" or "isolated clinic hypertension." It is defined as clinic or office blood pressure (BP) readings that are persistently higher than 140/90 mm Hg in conjunction with daytime ambulatory BP readings persistently lower than 135/85 mm Hg (the out-of-office BP equivalent of a clinic BP measurement of 140/90 mm Hg).

A 54-year-old woman with a history of hypertension presented with a worsening headache and a left hemisensory defect. A CT scan of her head without contrast showed a right parietal hemorrhage with spreading edema; the masslike effect caused shifting of the midline to the contralateral side. The patient gradually became comatose and required intubation for airway protection. Intravenous corticosteroids were administered to decrease the effect of the lobar hemorrhage. Fever developed 3 days after admission.

A morbidly obese 63-year-old woman with type 2 diabetes mellitus and hypertension presented with postmenopausal vaginal bleeding. A uterine biopsy revealed papillary mucinous adenocarcinoma, and biopsy of a breast mass detected during the examination also showed adenocarcinoma. The patient underwent irradiation of the pelvis and breast.

Abstract: Prompt correction of hypoxemia is a basic goal in the treatment of critically ill patients. Improvements in global oxygen delivery may be achieved by several means, such as providing an adequate fraction of inspired oxygen and using packed red blood cell transfusions for volume resuscitation. Low levels of positive end-expiratory pressure often help improve arterial oxygen tension. Measurement of mixed venous oxygen saturation (Sv?248-175?O2) can be useful in patient assessment. Sv?248-175?O2 may be decreased in patients with hypoxemia, hypovolemia, or anemia and may be elevated in patients with sepsis. Serum lactate levels may not quantitate the degree of tissue hypoxia, but serial measurements can help monitor the patient's response to therapy. For patients with septic or hypovolemic shock, early fluid resuscitation with isotonic crystalloid solution is essential. Catecholamine vasopressors can be useful when fluid administration fails to restore adequate blood pressure. (J Respir Dis. 2005;26(5):209-219)

A 65-year-old woman with well-controlled hypertension comes in for a routine checkup. During the past 10 years, she has gained 25 lb and lost 1.5 inches in height.

A 71-year-old woman presents to the emergency department accompanied by her daughter. The patient woke up in the morning "feeling fine" and then complained of a headache. She became progressively less oriented over the next 45 minutes.

Is there a role for statins in the treatment of chronic progressive renal disease?Inflammation is a component of the pathophysiology of progressive renal disease and may also be associated with other major modifiable risk factors, such as atherosclerosis, hypertension, and diabetes mellitus.

Cardiovascular disease is a leading cause of death in patients with chronic obstructive pulmonary disease (COPD). While some physicians may be reluctant to prescribe ß-blockers for these patients, because of concern about adverse effects on lung function, a study conducted by Au and associates indicates that ß-blockers may have an edge over other antihypertensive agents in reducing mortality risk.

How important is control of obesity in the treatment of hypertension?

A 35-year-old woman who is pregnant for the first time has had elevated blood pressure since she first presented for prenatal care at 28 weeks gestation.

An 83-year-old woman with a history of mild dementia and hypertension presented with rectal bleeding. Her husband stated that she had "hemorrhoids." Her current medications included donepezil, ramipril, and docusate sodium. Earlier in the year, a colonoscopy had revealed diverticulosis.

My patient is a 52-year-old woman with elevated levels of both low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol. She does not have a family history of cardiovascular disease; has never smoked; is of normal weight; and does not have diabetes, hypertension, or known atherosclerotic disease.
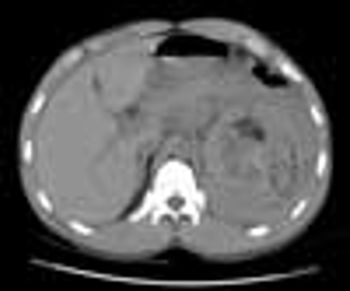
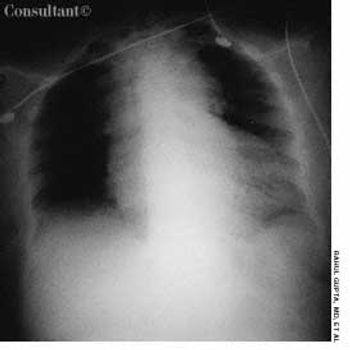
A 45-year-old man presented to the emergency department with severe left flank pain, tachycardia, and hypotension of about 48 hours’ duration. He had no significant medical history. His heart rate was 106 beats per minute; his blood pressure was 90/70 mm Hg. Laboratory results were notable for a hemoglobin level and a hematocrit in the lower end of the normal range.

For 2 years, a 79-year-old man had postprandial fullness and epigastric discomfort. He also experienced regurgitation and substernal pain after eating that was relieved by belching. He had a history of hypertension and gout. The patient’s vital signs were normal. Laboratory test results were within normal limits.

For 2 years, a 79-year-old man had postprandial fullness and epigastric discomfort. He also experienced regurgitation and substernal pain after eating that was relieved by belching. He had a history of hypertension and gout. The patient’s vital signs were normal.

A 58-year-old man with type 2 diabetes mellitus and hypertension was hospitalized with acute diarrhea characterized by several brown, liquid depositions per day. He also complained of lower abdominal pain and bloating and a 10-lb weight loss in the past 2 months. He denied fever or chills, use of corticosteroids, and travel outside the United States.