
US consumption of red meat remains twice the global average. New research highlights the consequences of that intake in terms of all-cause mortality.

US consumption of red meat remains twice the global average. New research highlights the consequences of that intake in terms of all-cause mortality.
A new study finds that higher caffeine intake may decrease the risk of patients developing new onset atrial fibrillation.
Saturated fat and cholesterol from red meat have long been known to be bad for heart health, but recent research sheds light on a possible new culprit.

In this older patient with T2DM, HFpEF, and other comorbidities, which class of medication is most appropriate--and guideline-recommended?

The new "sweet spot" in diabetes management is the interdisciplinary approach that is essential to treating all aspects of the disease. New diabetes medications also hit that spot.

ADA 2019--Linagliptin, the DPP-4 inhibitor, showed similar risk for first or recurrent CV events or hopspitalization vs placebo in T2DM patients with high cardiorenal risk in CARMELINA subanalysis.
ADA 2019-Dapagliflozin reduced CV death, hospitalization for HF, and progression of CKD among T2DM patients with a wide distribution of baselines CVD risk in DECLARE-TIMI 58.

Patients know that regular exercise is important but often need guidance on what's best. A pulmonologist advises on how to asses individual needs, utilize guidelines, and create a plan.
A personal EKG monitor, an app that wirelessly connects to a smart thermometer, and 3 more FDA-cleared apps for primary care.
Test your knowledge of the key elements and outcomes of the highly buzzed about REDUCE-IT trial with this 5-question quiz.
Eighty percent of all cardiovascular events are preventable. The ACC/AHA 2019 guidelines are a single source of best practices to help achieve that goal. Review them here, at-a-glance.

From a mobile EKG monitor to a digital urinalysis app, these medical "devices" are changing the way healthcare is delivered.

Dapagliflozin, icosapent ethyl, and bempedoic acid were found to reduce clinical or surrogate CV endpoints in studies presented at ACC.19, March 16-18, in New Orleans, LA.
Find out what you know about which diabetes drugs in which classes show CV protective properties and results of the trials that support their use.

Psoriasis medication for heart disease prevention, the role of artificial sweeteners in different types of stroke, and 3 other noteworthy findings from American Heart Month.
What approach is now AHA/ACC guideline-recommended for a patient with primary hypercholesterolemia, with an LDL-C of 192 mg/dL? Take Quiz #3.
From a mobile fluid tracker to an app with a 3-D beating heart, these are the top 5 heart failure apps that every primary care physician and patient should know about.
How will changes in the AHA/ACC update to the 2013 guidelines help optimize care for patients with ASCVD? Try part 2 of our 3-part quiz and find out.
What's new and what's not in the AHA/ACC 2018 update to the 2013 lipid management guidelines? Try part I of our 3-part quiz and find out.
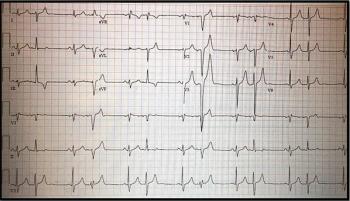
Other than sleep problems, this 52-year-old has no other medical history. What's your ECG read? Does the computer assessment agree?
As the new year begins, several developments in heart health research are making the news.
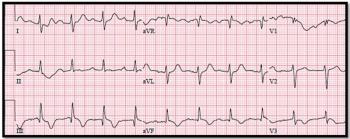
The 82-year-old is observed to be in respiratory distress but denies any symptoms. See the ECG for more information. Your dx?
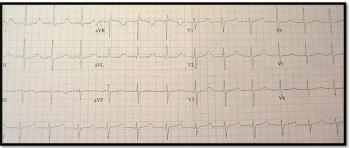
The 32-yr-old claims no medical history other than "thyroid surgery" and takes no medications. What does the ECG suggest?

What impact does this highly purified form of omega-3 fatty acid have on cardiovascular events? Authors of the REDUCE-IT trial sought to find out.
Under what circumstance/s is it appropriate to initiate treatment for hypertension with a single drug (followed by titration, additional agents)?