
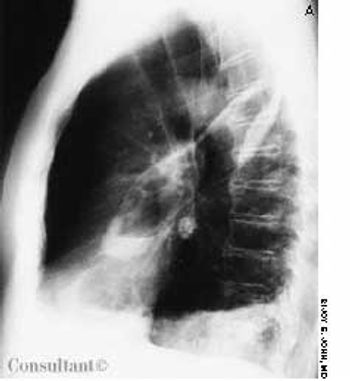
A 59-year-old man presented with a cough and 2 episodes of pneumonia during the past 4 months. He had a 45-pack-year history of smoking cigarettes.


A 59-year-old man presented with a cough and 2 episodes of pneumonia during the past 4 months. He had a 45-pack-year history of smoking cigarettes.

A 29-year-old man presented with a complaint of venereal warts and a long history of mild psoriasis, which he had treated with fluocinolone. He returned 3 months later complaining of chest congestion of 10 days' duration; it had been treated with ciprofloxacin at an urgent care facility.
A 70-year-old man-nursing home resident-had had a cough, fever, and copious foul-smelling sputum for 1 week. Hemoptysis was noted off and on during the previous 3 days. The patient had no recent weight loss. A chest x-ray film and a CT scan showed an air-fluid level in the left oblique fissure of the lung as well as pleural thickening and infiltrates in the left lower zone.

How do you assess the likelihood of antibiotic resistance in patients presenting with suspected pneumococcal infection? Vanderkooi and associates addressed this in a study of 3339 patients with invasive pneumococcal disease. They found that antibiotic use in the 3 months before the onset of infection was the most important risk factor for antibiotic resistance. The single most important risk factor for resistance to a particular antibiotic was previous use of antibiotics from the same class.

Abstract: The idiopathic interstitial pneumonias (IIPs) are the most commonly diagnosed forms of interstitial lung disease. These diseases represent specific clinicopathologic entities characterized by varying degrees of lung parenchymal inflammation and fibrosis. While most patients present with chronic dyspnea and have evidence of restriction on pulmonary function testing, certain findings can help differentiate among the IIPs. For example, patients with idiopathic pulmonary fibrosis (IPF)--the most common IIP--commonly present in the sixth or seventh decade of life, while those with desquamative interstitial pneumonia or respiratory bronchiolitis with interstitial lung disease typically present in the third or fourth decade of life and have a history of smoking. IPF is characterized by usual interstitial pneumonia (UIP) on lung biopsy; a UIP pattern can also be identified by high-resolution CT. (J Respir Dis. 2005;26(9):372-378)

A 67-year-old woman was referred for evaluation of exertional dyspnea, with multiple episodes of fever, cough, and pneumonia. She had a long history of cough with sputum and had been admitted several times for exacerbations of chronic obstructive pulmonary disease and pneumonia. She received maintenance therapy with an ipratropium and albuterol combination, fluticasone, and salmeterol, but she continued to experience exertional dyspnea, with an average of 5 or 6 exacerbations and 2 hospital admissions a year.

This painless, bleeding lesion had developed insidiously on the penis of a 47-year-old HIV-positive man. The patient was inconsistently compliant with antiretroviral therapy. He had a history of Pneumocystis carinii pneumonia and widespread cutaneous Kaposi sarcoma. The 2.5-cm, friable but firm, exophytic nodule was on the distal shaft of the penis.

Abstract: The standard therapies for acute exacerbations of chronic obstructive pulmonary disease include short-acting bronchodilators, supplemental oxygen, and systemic corticosteroids. For most patients, an oxygen saturation goal of 90% or greater is appropriate. Bilevel positive airway pressure (BiPAP) is usually beneficial in patients with progressive respiratory acidosis, impending respiratory failure, or markedly increased work of breathing. However, BiPAP should not be used in patients with respiratory failure associated with severe pneumonia, acute respiratory distress syndrome, or sepsis. Systemic corticosteroids are appropriate for moderate to severe acute exacerbations; many experts recommend relatively low doses of prednisone (30 to 40 mg) for 7 to 14 days. Antibiotic therapy is controversial, but evidence supports the use of antibiotics in patients who have at least 2 of the following symptoms: increased dyspnea, increased sputum production, and sputum purulence. (J Respir Dis. 2005;26(8):335-341)

The authors describe a case of acute eosinophilic pneumonia (AEP) that occurred in a previously healthy young man. The presentation was similar to that of acute respiratory distress syndrome (ARDS), and the diagnosis was established by bronchoalveolar lavage (BAL). The authors note that it is important to recognize the subset of patients with AEP who present with an ARDS-like picture, especially since corticosteroids are very effective in this setting.

While acute Q fever can cause pneumonia and other febrile illnesses, it is often asymptomatic. You may want to consider testing for Q fever if a patient is infected with another tick-borne pathogen, according to a report by Rolain and associates. They described 6 patients infected with organisms such as Rickettsia conorii who also were infected with Coxiella burnetii, the cause of Q fever.

A 54-year-old woman with a history of hypertension presented with a worsening headache and a left hemisensory defect. A CT scan of her head without contrast showed a right parietal hemorrhage with spreading edema; the masslike effect caused shifting of the midline to the contralateral side. The patient gradually became comatose and required intubation for airway protection. Intravenous corticosteroids were administered to decrease the effect of the lobar hemorrhage. Fever developed 3 days after admission.

The American Thoracic Society (ATS) and the Infectious Diseases Society of America recently published guidelines for the management of hospital-acquired pneumonia (HAP).1 These guidelines, which are an update of a 1996 ATS consensus statement,2 focus on bacterial HAP in immunocompetent adults. This includes ventilator-associated pneumonia (VAP) and health care-associated pneumonia (HCAP). Selected highlights are presented here.

In their Photoclinic case of a man with achalasia (CONSULTANT, February 2005, page 268), Drs Sonia Arunabh and Manjula Thopcherla did not mention the extensive abnormalities evident in the left lung on both radiograph and CT .Did the patient also have aspiration pneumonia?

Just how effective are the national guidelines for the management of community-acquired pneumonia (CAP)? Pretty good, according to Mortensen and associates. They found that compliance with practice guidelines, such as those published by the Infectious Diseases Society of America and the American Thoracic Society, is associated with a reduced mortality in patients with CAP.

Although pneumonia caused by Legionella pneumophila continues to be associated with significant morbidity, recent studies indicate that the mortality rate has declined. Two studies from Spain support this observation and suggest that therapy with levofloxacin may be more effective than therapy with erythromycin or clarithromycin.

Abstract: The use of sputum studies and blood cultures in patients hospitalized with community-acquired pneumonia (CAP) is somewhat controversial, and recommendations continue to evolve. A reasonable approach is to attempt to obtain sputum cultures from all patients before initiating antibiotic therapy. If antibiotics have already been given, sputum studies can be reserved for patients who are severely ill or who are at risk for infection with a resistant organism or an organism that is not covered by the usual empiric therapy. The Infectious Diseases Society of America and the American Thoracic Society both recommend obtaining blood cultures from all patients. However, cost considerations have led to alternative strategies, such as reserving blood cultures for those with severe CAP. (J Respir Dis. 2005;26(4):143-148)

A 67-year-old woman underwent right pneumonectomy for non-small-cell carcinoma of the right lung. Her postoperative course was uneventful, and she was discharged from the hospital on the fifth day.

A 69-year-old woman was hospitalized with fever, chills, and nausea. Three weeks earlier, she had received a 2-week course of oral levofloxacin for pneumonia, which resolved. Her history included rheumatic heart disease; diabetes mellitus; depression; a hysterectomy; 2 mitral commissurotomies; nonrepairable mitral valve regurgitation, for which she received a St Jude Medical bileaflet valve; a left-sided cerebrovascular accident; and paroxysmal atrial fibrillation. Her medications included verapamil, furosemide, metoprolol, potassium chloride, metformin, nortriptyline, and warfarin. She denied tobacco and alcohol use.

ABSTRACT: The rate at which acute dyspnea develops can point to its cause. A sudden onset strongly suggests pneumothorax (especially in a young, otherwise healthy patient) or pulmonary embolism (particularly in an immobilized patient). More gradual development of breathlessness indicates pulmonary infection, asthma, pulmonary edema, or neurologic or muscular disease. A chest film best identifies the cause of acute dyspnea; it can reveal pneumothorax, infiltrates, and edema. Pulmonary embolism is suggested by a sudden exacerbation of dyspnea, increased ventilation, and a drop in PaCO2. A normal chest radiograph reinforces the diagnosis of pulmonary embolism, which can frequently be confirmed by a spiral CT scan of the chest. Pneumonia can be difficult to distinguish from pulmonary edema. In this setting, bronchoalveolar lavage and identification of the infectious organism may be necessary to differentiate between the 2 disorders.

35-year-old Hispanic man presented with nonproductive cough; dyspnea; fever; and a painful, ulcerated, 1.5-cm, red-brown plaque on the left flank. He had had the lesion for 3 months and the symptoms for 1 week. The patient had grown up in Arizona, and he traveled there 4 months before the lesion arose.

A52-year-old white man presented with a pruritic eruption on the neck of 3 months’ duration. The rash had not responded to a potent topical corticosteroid prescribed by another practitioner for the presumed diagnosis of eczema. The patient reported no current health problems. His history included a pubic louse infestation and several episodes of uncomplicated urethral gonorrhea. He readily admitted to having unprotected sexual intercourse with prostitutes.

An 85-year-old man was admitted to the hospital with acough and shortness of breath of 1 week’s duration anda fever and increased sputum production for 2 days. Hishistory included renal cell carcinoma and metastatic renalcancer for 2 years. The patient had smoked cigarettesfor 30 years. He had lost 30 lb during the last few months.A chest film revealed pneumonia of the right lowerlobe. Metastatic nodules were noted on the scalp; extensivelung, bone, and brain metastases also were found.

ABSTRACT: A cough is considered chronic when it persists for 3 or more weeks. Typically, chronic cough is a lingering manifestation of a viral upper respiratory tract infection; other, more serious causes-such as asthma, sinusitis, or gastro- esophageal reflux-must also be considered. Look to the history for diagnostic clues and order a chest film, which may point to pneumonia, hyperinflation, atelectasis, or cardiac or pulmonary abnormality. Diagnostic test methods will depend, in part, on the child's age; for example, the American Academy of Pediatrics recommends against imaging of the sinuses in children 6 years or younger. Pulmonary function tests can be useful in diagnosing asthma if the child is able to cooperate. Consider ordering a barium swallow for a very young child whose cough may be the result of a vascular anomaly. A pH probe study can help you determine whether cough is secondary to gastroesophageal reflux. Treatment is directed at the underlying cause.

In November 2002, cases of an atypical pneumonia were reported in the Guangdong province of southern China. By the following June, outbreaks of the illness-known as severe acute respiratory syndrome (SARS)-had occurred in Germany, Ireland, the United States, Canada,Hong Kong,Singapore, and Vietnam.
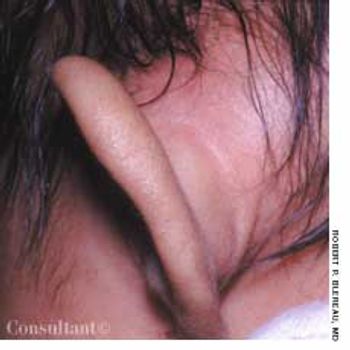
Concerned that her 7-week-old daughter's left ear was far more prominent than the right one, the mother took the infant to the emergency department (ED) for evaluation. The swelling had begun 3 or 4 days earlier; the patient was otherwise asymptomatic.