
Skin signs of systemic disease: sarcoidosis, rheumatoid nodules, Muir-Torre syndrome, diabetic vasculopathy, hyperlipidemic nodules, zinc deficiency, and Sister Mary Joseph nodule.

Skin signs of systemic disease: sarcoidosis, rheumatoid nodules, Muir-Torre syndrome, diabetic vasculopathy, hyperlipidemic nodules, zinc deficiency, and Sister Mary Joseph nodule.

Statins (HMG-CoA reductase inhibitors) are the most effective drugs in the management of elevated low-density lipoprotein cholesterol (LDL-C) levels. Recent large clinical trials continue to demonstrate the remarkable efficacy of these agents, including improved outcomes.

The metabolic syndrome represents a clustering of conditions and/or risk factors that lead to an increased incidence of type 2 diabetes mellitus and cardiovascular disease. These conditions include abdominal obesity, dyslipidemia, hypertension, insulin resistance, and a proinflammatory state.

A 56-year-old woman was referred for management of severe hyperlipidemia. Her family history included hypercholesterolemia and premature coronary artery disease.

A 36-year-old man was admitted to the hospital with acute mid-epigastric pain and vomiting. He was a heavy drinker and had smoked between 50 and 60 cigarettes a day for the last 15 years.

A male infant was born to a 29-year-old woman (gravida 3, para 2), following an uncomplicated pregnancy and normal vaginal delivery. At birth, a brownish 1-cm nodule was noted on the right side of the upper abdomen. The infant was otherwise healthy.

A 65-year-old man presented with bluish toes and petechiae on his toes and feet 3 days after having undergone renal angiography. Bilateral pitting pedal edema was noted, and laboratory tests revealed proteinuria, eosinophilia, and an erythrocyte sedimentation rate (ESR) of 65 mm/h.

A 56-year-old man was admitted to the hospital with right lower lobe pneumonia, which was exacerbated by smoking-induced chronic obstructive pulmonary disease (COPD).

An 85-year-old white woman was brought to the emergency department (ED) with acute, severe left posterolateral chest wall pain of several hours' duration. The nonradiating pain was accompanied by shortness of breath. She denied palpitations, diaphoresis, syncope, or dizziness.
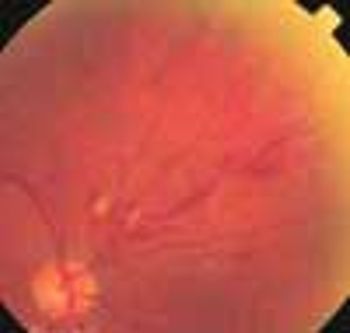
A dilated and tortuous vein, flame-shaped hemorrhages, dot-blot hemorrhages, and cotton-wool spots (retinal ischemia) that extended along the supranasal retinal arcade of the right eye were found during a 73-year-old man's annual eye examination. Because these changes were isolated to one quadrant and did not involve the macular area, the patient had no symptoms.

A 49-year-old woman noticed a growing lesion near the inner corner of her left upper eyelid. The lesion had become conspicuous because of its size and color; the patient wanted it removed.

Four months after coronary artery bypass surgery, a 77-year-old man began to suffer severe pain in his feet. Multiple necrotic areas developed on the toes.

For 1 week, a 22-month-old boy experienced gradually increasing facial swelling followed by swelling of the abdomen and legs. His mother reported that the child's urinary output had markedly decreased. During this period, the youngster gained 5 lb.

A 51-year-old woman complained of mild pain in the Achilles tendon area of both feet. This was aggravated when she stood for prolonged periods and when she wore tight, high-heeled shoes. Physical examination results were unremarkable except for a disputable palpable thickness of the Achilles tendons, especially on the right foot.

For years, cardiologists and primary care physicians have engaged in a spirited debate about the appropriate target for low-density lipoprotein cholesterol (LDL-C) lowering in patients with coronary artery disease.

These yellow asymptomatic lesions on the inner upper eyelids of a 36-year-old woman had persisted for 2 years. She had a history of type 2 diabetes mellitus, migraine, nicotine dependence, bipolar disorder, and obesity. Her medications included quinapril, insulin aspart injection, sumatriptan, ziprasidone, and temazepam.

The parents of a 16-year-old girl report that during the past several months, she has exhibited behavioral changes, irritability, increased anger, depression, and anxiety. The girl had previously been healthy, and there has been no recent illness or trauma.

A tender nodule; an itchy truncal rash; multiple pruritic eruptions--can you identify the disorders pictured here?

Inflammation plays a major role in coronary artery disease (CAD), whereby inflammatory changes develop in the blood vessel walls.1 This observation has spurred interest in exploring the connection between CAD and markers of inflammation, including C-reactive protein (CRP), fibrinogen, serum amyloid A, and many other novel markers.

During a routine annual checkup, a 5-ft 8-in, 94.5-kg (210-lb) 13-year-old girl was noted to have a hyperpigmented "dirty" lesion on the back of her neck. The girl's parents were also obese. Her mother had type 2 diabetes mellitus.

One third of all American adults (more than 70 million people) are currently on a diet. More than half of all adults have attempted dieting at some point--often more than once.

I would like to offer a few comments on the reply by Dr Michael Prisant to a reader's question about whether statin therapy is appropriate for a 52-year-old woman with a high low-density lipoprotein (LDL) cholesterol level and a high high-density lipoprotein (HDL) cholesterol level

How much fish oil should I recommend that my patients with heart disease take?

As recommended by the authors, I commonly order a fasting lipid profile and measurements of glucose and insulin levels in children at risk for type 2 diabetes. One area of management that remains confusing is the approach to take with children who have an elevated fasting insulin level but otherwise normal laboratory results.

Several popular diets, such as the South Beach Diet and Sugar Busters, are based on the glycemic index; however, many patients are confused about its significance.