
A recent white paper declares it time to abolish the ambiguous term. Given current knowledge of atrial fibrillation, the 60-year-old description serves only to confuse.

A recent white paper declares it time to abolish the ambiguous term. Given current knowledge of atrial fibrillation, the 60-year-old description serves only to confuse.

The United States Preventive Services Task Force narrows recommendations for populations that warrant screening. Guideline revisions are based on a new evidence review.

The science behind the dangers of testosterone therapy is called into question by researchers who find the outsized reaction to flawed data counterproductive for physicians and patients alike.
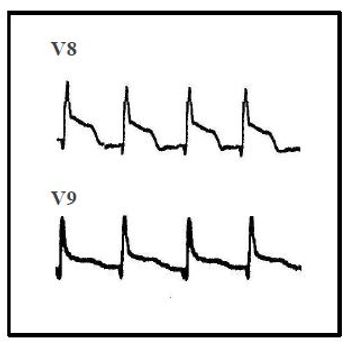
The patient describes acute onset of chest pain with nausea and diaphoresis. The cardiac and pulmonary examinations are normal. What does the 12-lead ECG reveal?


Aging baby boomers will more frequently appear in primary care offices with cardiovascular diseases that place them at high risk for both clotting and bleeding. Many will also have atrial fibrillation. Is there a sure-fire therapeutic formula for all?

In a clinical trial setting, performance of the new oral anticoagulant and the long-time gold standard was similar. In the real world, where adherence can be a problem, there is a risk/benefit ratio to consider.
Optimal therapy of neuropathic pain? Optimal anticoagulation with a mechanical aortic valve? What’s the significance of a positive Hoffman sign? See if you can answer these and 2 other of our quiz questions.

An extensive meta-analysis calls into question the standard practice of switching from an ACEI to an ARB in patients with type 2 diabetes.

The exact mechanism responsible for this effect is still open for debate. A salutatory side effect of the news may be the impact on medication adherence among men with both elevated LDL-C and erectile dysfunction.
This 32-year-old woman's family brought her to the ED after 2 days of progressive confusion, fatigue, and weakness. Her multiple medical problems included juvenile-onset diabetes mellitus. Here, more details and a management challenge.

Hyperkalemia is the most serious of the electrolyte disorders and can lead to death if not managed appropriately.

If common mechanisms underlying cryptogenic stroke can be clarified, we will need to reevaluate the current approach to secondary prevention. Here, elucidation of "emoblic stroke of undetermined source."

Group-based lifestyle interventions have long-term effects on prevention of diabetes beyond the period of active intervention, this clinical trial shows.

This finding could encourage more men with cardiovascular disease to remain compliant with their therapy.

Good cardiovascular health may help preserve memory and thinking skills into middle age, according to the results of a new study.

Americans’ average daily sodium intake may be associated with better health outcomes than recommended intake levels.

Two new studies show the heart-healthy benefits of this eating plan.
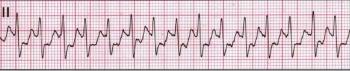
The patient denies dizziness, weakness, chest pain, and dyspnea. Review case details including ECG results. What's your diagnosis?

Management options for PSVT in a stable patient include vagal maneuvers, medications, and electrical synchronized cardioversion.

The benefits of statin therapy no longer stand uncontested as they did early in the life cycle of the class. The pro and con camps each can point to science, but in the end it's about personalized medicine.

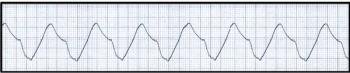
A wide-ranging meta-alaysis found that brief, intense outbursts of anger triggered onset of acute myocardial infarction, acute coronary syndrome, and dangerous ventricular arrhythmias.

The authors investigated changes in specific proinflammatory genes associated with neutrophil activation in patients with known coronary artery disease or with significant risk factors.

In clinical scenarios where warfarin is still the drug of choice for anticoagulation, it is still a challenge to achieve optimal time in therapeutic range. Is there promise in a new dosing paradigm?

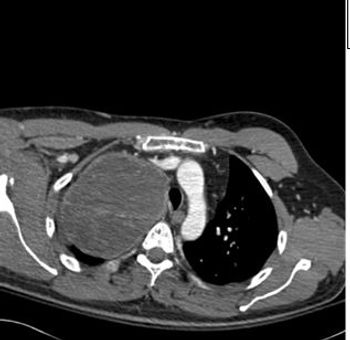
Results of a new study suggest that number of LAA lobes may one day be useful as an element of the CHADS2 scoring system for embolic risk in patients with atrial fibrillation.