
“Stippled” pigment is highly typical of a pigmented basal cell carcinoma. Diagnostic contenders include atypical seborrheic keratosis and superficial spreading melanoma.

“Stippled” pigment is highly typical of a pigmented basal cell carcinoma. Diagnostic contenders include atypical seborrheic keratosis and superficial spreading melanoma.

The morphology of a round, red to purple patch, with or without blistering, is typical of a fixed drug eruption. This entity usually manifests as a solitary spot, but can be multiple. Tetracycline antibiotics and barbiturate sedatives are common causes. This patient had been taking doxycycline.

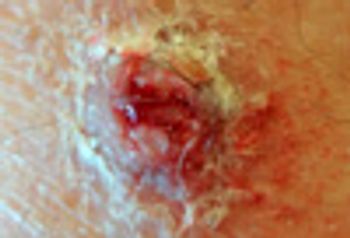
This friable lesion with rapid and destructive growth is classic for granuloma inguinale. This patient was treated successfully with trimethoprim/sulfamethoxazole.

Condylomata acuminata this extensive are beyond the capacity of all topical therapies. The area was initially treated by carbon dioxide laser ablation, and residual small foci of infection were subsequently treated with topical 5% imiquimod cream.

The combination of itching massive scaling suggests the diagnosis of crusted scabies. This variety of scabies is seen in those who are immunosuppressed or immunocompromised (typically HIV+). Repeated oral doses of ivermectin along with topical permethrin application were required to clear this infestation.

A 24-year-old woman sought medical attention because of the acute onset of a very painful vulvar rash. She had never experienced anything similar. Do you recognize these lesions?

This teen sought care because of extremely pruritic nodules on the penis and scrotum. He also had mild itching on the wrists and between several finger webs. This distribution of a pruritic dermatosis is classic for scabies.

The patient received standard acyclovir dosage for first outbreak genital herpes: 200 mg orally, 5 times daily, for 10 days total. At this point, there is no way to predict how often or how severe future recurrences will be.

This painless, indurated ulcer is typical of the chancre of primary syphilis. This patient also had a positive RPR in a titer of 1:32.

Any adult with patchy hair loss with preservation of follicular openings should be questioned about sexual exposures. This presentation is not typical of alopecia areata, and the patient is too old for tinea capitis to be a major consideration.

Chlamydia trachomatis, serovar L2b-a recently discovered microbe-was the cause of atypical lymphogranuloma venereum in this HIV-positive patient.

This multi-factorial eruption requires topical or systemic antifungal treatment in conjunction with broad-spectrum antibacterial therapy, topical desiccating maneuvers (such as Burrow’s soaks), and discontinuation of OTC interventions that might be worsening the problem.

Squamous cell carcinoma is the most common tumor of the penis. Melanoma, sarcoma, and (rarely) basal cell carcinoma and cutaneous metastasis also occur here.

The confluence of small, scaly, hyperpigmented patches on the chest (and often neck and upper back) is classic for tinea versicolor.

These firm, pigmented plaques, in a young African American, are most likely cutaneous sarcoidosis. This diagnosis was verified by biopsy.

The patient was a traveling salesman and was concerned that the lesions were bedbug bites. The diagnosis of herpes simplex virus infection was confirmed by viral “culture.” What was this patient's condition?

There is a rather large erythematous patch/plaque present. However, an exophytic, verrucous nodule is visible at the inferior border of the tumor. Biopsy of the flatter portion of this lesion disclosed squamous cell carcinoma in-situ, while biopsy of the nodule revealed invasive squamous cell carcinoma.

One of two common presentations of tinea pedis, this morphology is more common in those whose interdigital space is tight, leading to moisture retention and maceration. Diligent use of any topical antifungal will clear this.

The 2% preparation of an allylamine antifungal is a new addition to the menu of available topical agents. It has the advantage of once-daily dosing and shorter course of therapy.

A 57-year-old man presented for medical evaluation because of the presence of a "funny looking lump" on the lateral aspect of his right upper thigh.
An 88-year-old woman sought medical attention for a nodule on the anterior surface of her left foreleg that had gradually developed.

This large bruise developed after the patient had an accident in her yard. Post-traumatic subcutaneous hematomas are common in elderly women, especially those who are anticoagulated. Untreated, the hematoma can eventuate into an abscess and even sepsis.

This lesion looks like basal cell or squamous cell carcinoma, but biopsy showed it to be an idiopathic inflammatory disorder of the external ear. Skin cancers of the pinna are rarely painful, as this lesion was.

This uncommon benign entity closely mimics squamous cell carcinoma, superficial basal cell carcinoma, and advanced actinic keratoses. The lichenoid keratosis does not transform into skin cancer.

The only impressive thing about this lesion was a “notch” in its superior pole, and some mild pigment heterogeneity. Prudent caution proved extremely beneficial. The history of a “new” lesion in a patient with almost no visible nevi, along with some very subtle gross features, led to early recognition and elimination of a malignant melanoma.

It is often surprising how wide and how deep skin cancers have already spread, despite a relatively small-looking superficial component. This patient had a history of melanoma in situ.

Consider all relevant factors when deciding what steps to take with a pigmented lesion noticed by the patient or encountered during a routine physical examination.

Almost no benign disorder affecting nasal skin should bleed.

Always check the toenails for fungal infection after diagnosing tinea pedis, corporis, or cruris. The toenails may act as the source of infection and a reservoir, which may lead to reinfection after the cutaneous dermatophytosis is cleared.

The eccentric placement of a darker spot within the overall lesion should raise suspicion for melanoma. This lesion’s asymmetry is the most worrisome feature. The need for histologic examination is clear in such cases.