New Spin on Hypertension: Sequelae of Excess Glucocorticoids and Mineralocorticoids
Persons with primary hyperaldosteronism and hypertension are at significantly increased risk for cardiovascular morbidity and mortality. But if these patients are treated with spironolactone and reach target blood pressure, their CV outcomes are the same as those of others with essential hypertension after 6.5 years of follow-up.
Contemporary hypertension management differentiates between hypertension and “resistant” hypertension. To label hypertension resistant, an optimally dosed 3-drug regimen that includes a diuretic must fail to achieve target blood pressure.
It is not surprising that people with resistant hypertension have more cardiovascular morbidity and mortality. Their blood pressure is higher on average, and not at target. But, did you know that glucocorticoid- or mineralocorticoid-dependent hypertension increases complications-regardless of whether it is resistant? A recent review delineates problems unique to steroid-driven hypertension.1
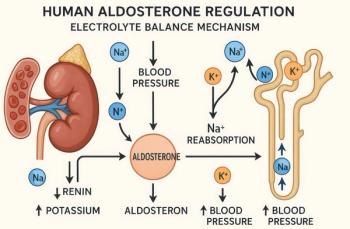
First, a brief exploration of the pathophysiology of primary hyperaldosteronism (PA). The prevalence of this entity increases with the severity of hypertension. In a cohort exceeding 600 patients, for example, the prevalence of PA was 2% in those with stage 1 hypertension; in those with stage 2 and stage 3 hypertension, PA prevalence increased to 8% and 13%, respectively. In patients with resistant hypertension, 20% may be under the dangerous influence of excess aldosterone.
Persons with PA and hypertension are 4 times more likely to have had a stroke, 6.5 times more likely to have had a myocardial infarction, 2 to 3 times more likely to have ECG-discovered left ventricular hypertrophy, and a whopping 12 times more likely to have atrial fibrillation. But, here is a key statistic: if these patients are treated with spironolactone and reach target blood pressure, after approximately 6.5 years follow-up, their cardiovascular outcomes are the same . . . no longer worse . . . as those of other patients with essential hypertension.
Data have demonstrated that aldosterone increases LV hypertrophy out of proportion to blood pressure. Antagonizing aldosterone’s deleterious effects, either by adrenalectomy or spironolactone, can improve or reverse cardiac end-organ damage.
Glucocorticoid effects, either from endogenous or exogenous steroids, can also raise blood pressure. Glucocorticoid-mediated hypertension increases risks for heart failure. Even doses that are not typically considered therapeutic, 7.5 mg of prednisone, for example, can increase cardiovascular events by as much as 2.5 times. Glucocorticoids compound hypertension’s complications through insulin resistance and metabolic syndrome.
How should these data inform primary care practice?
1. When a patient does not reach target blood pressure on an optimal 3-drug regimen, think of secondary causes and use spironolactone when appropriate.
2. Screening for excess aldosterone is simple and noninvasive. An aldosterone to renin ratio of 30:1 or greater suggests aldosterone excess.
3. A 24-hour urine for free cortisol, a dexamethasone suppression test, or a salivary cortisol (if available) can be used to screen for Cushing disease.
4. Since excess corticosteroids and mineralocorticoids not only cause hypertension, but also accelerate CV complications, they should be considered in select patients with hypertension (especially those with resistant hypertension) and treated accordingly. Spironolactone is inexpensive and may be lifesaving.
Reference
1. Pimenta E, Wolley M, Stowasser M. Adverse cardiovascular outcomes of corticosteroid excess. Endocrinology. 2012 Aug 23; [Epub ahead of print].
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.