Late Breakers in Atopic Dermatitis: Highlights and Previews with Alexandra Golant, MD
From the revolutionary approval of dupilumab to the promise of potential disease modification with OX40 inhibitors, Golant provided a wide-ranging update of the treatment space.
"We know atopic dermatitis is kind of hot now. It hadn't been before the last 10 years or so, because we didn't have great therapeutics. But now, we've entered a period of rapid therapeutic revolution in AD. What did 2024 bring? What will 2025 continue? Let's dive in."
With that, Alexandra Golant, MD, began a review of the state of the art in treating atopic dermatitis as well as a preview of the future, touching on the medications in the pipeline that address novel disease targets and reflect what she referred to as "dipping a toe" into disease modification. She made her presentation, Late Breakers in Atopic Dermatitis, at the 2025 At the 2025 Midwinter Clinical Hawaii Dermatology Conference, held February 15-29, 2025, on the Big Island, Waikoloa Village, HI.
Golant is the medical director of the faculty practice and the associate program director for the residency program in the department of dermatology at the Icahn School of Medicine at Mount Sinai, in New York.
Understanding the Complexity of Atopic Dermatitis
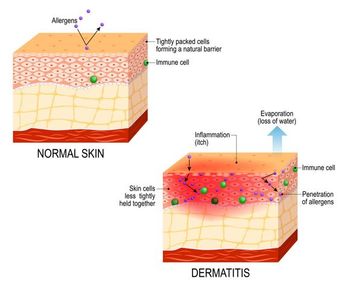
"AD is a highly heterogeneous disease. No two patients look exactly alike,” Golant said, noting that it varies by patient age, skin phenotype, and lesion chronicity. While type 2 inflammation predominates, other immune pathways also play critical roles in disease pathogenesis, which helps explain the differential effect of therapeutics across patient populations.1
Recent research has highlighted increased rates of comorbidities with AD, “and not just atopic ones like asthma but others like osteoporosis, vitiligo, and alopecia areata that all occur at greater rates in our patients with atopic dermatitis."2 A key question is: can early intervention modify these risks?” Golant said that early studies suggest that answer is “yes.” She described a retrospective analysis in children aged 6 to 11 years treated with dupiulmab that showed rapid normalization of bone mineralization biomarkers within 16 weeks.3 “This is exciting because it may fundamentally change the narrative for our youngest patients and potentially interrupt the atopic march."
Updated Guidelines for Disease Severity and Systemic Therapy
Revised guidelines from the American Academy of Dermatology (AAD) define moderate-to-severe AD by a minimum body surface area (BSA) involvement of 10% or by high-impact areas (eg, face, genitals, palms/soles) and significantly impaired quality of life.4 Golant noted that it is usually clear when the topical agents are appropriate and they span the range for the patients with mild to moderate disease, and sometimes are valuable as adjunctive treatment to systemic therapy. In her next comments, she was adamant.
“I would implore you not to forget those moderate patients, those moderate patients who are kind of teetering on the edge of control, just getting by sometimes overusing topicals. Really focus on quality of life when you're seeing your patients in the clinic.
Remember, Golant said, these patients have been suffering with the disease for years and so modest improvement to them is going to feel significant—but it may not be the optimal response. “So, I really have honed in on asking about quality of life, asking about true disease control to understand when I'm going to have that conversation about escalating care. Don't reserve your systemic just for your worst severe patients, your moderate patients deserve them too.”5
Golant followed with snapshots of the research demonstrating the efficacy of all the current treatments for AD in the toolbox and in the pipeline, across mode of delivery, mechanism of action, phase of clinical study, and FDA approval status.
Topical Therapies: New and Emerging Options
Ruxolitinib Cream (JAK1/2 Inhibitor): The TRuE-AD3 study demonstrated robust efficacy in children aged 2 to 11 years, with 52-week data showing sustained IGA 0/1 (clear/almost clear) responses and a favorable safety profile.6 (FDA approved 2022)
Roflumilast Cream (PDE4 Inhibitor): Data from the INTEGUMENT-1/2 trials in patients aged 6 years and older showed significant improvements in vIGA-AD and pruritus by week 4, with durable efficacy through 52 weeks in the open-label extension.7 (FDA approved July 2024)
Tapinarof Cream (AHR Modulator): ADORING 1/2 trials demonstrated significant IGA success and pruritus reduction at week 8 in patients aged ≥2 years. This therapy allows proactive maintenance with intermittent use.8 (FDA approved December 2024)
Systemic Therapies: Expanding the Toolbox
"Let's move to systemics. Dupilumab was our first approved medication for AD and it drove a paradigm shift,” Golant said. “I tell my patients it is a once-in-practice-lifetime medication, because it changed everything about the atopic dermatitis space when it was approved.”
Dupilumab (IL-4Rα Inhibitor): Long-term data from the LIBERTY-AD-HAFT trial confirmed efficacy in chronic hand eczema. Additionally, a six-year retrospective analysis revealed a lower risk of internal malignancies in patients treated with dupilumab.9,10 (FDA approved 2017)
Tralokinumab (IL-13 Inhibitor): The ECZTEND study reported sustained EASI-75 responses (93%) through week 248, including efficacy in patients who previously failed dupilumab, with good response in head and neck AD.11 (FDA approved 2021)
"On to our new kids on the block.”
Lebrikizumab (IL-13 Inhibitor): Three-year data show sustained efficacy, with approximately 80% achieving EASI-90 at week 152.12 (FDA approved September 2024)
Nemolizumab (IL-31 Inhibitor): ARCADIA 1/2 trials confirmed rapid pruritus relief and durable efficacy with q4-8 week dosing.13 (FDA approved December 2024)
JAK Inhibitors: Speed of Response and Sustained Control
Upadacitinib (JAK1 Inhibitor): Integrated safety data over 5 years confirm a consistent safety profile, with superior pruritus and skin clearance compared to dupilumab in the HEADS-UP trial, the first head-to-head study with dupilumab.14 (FDA approved 2022)
“I want to comment here on the composite endpoint of EASI-100 and that itch free state – approximately 28% of the patients achieved that endpoint at week 16, and some of these were dupilumab nonresponders."
Abrocitinib (JAK1 Inhibitor): Label updates now allow dose escalation to 200 mg daily if the 100 mg dose is insufficient, supporting personalized treatment approaches.15 (FDA approved 2022)
The Future: Novel Targets and Disease Modification
“OX40 should be on your radar,” Golant urged. “It’s a really interesting pathway involved in T-cell activation and is going to be a new way to target this disease. And what is very interesting about the data is even when you withdraw, there seems to be a lingering effect. We're starting to dip the toe, some would say, into disease modification.”
OX40 Inhibitors: Amlitelimab (STREAM-AD phase 2 trial) and rocatinlimab show sustained efficacy after treatment cessation, suggesting potential disease modification.16
IL-22 and IL-18 Pathways: Emerging data on temtokibart (IL-22RA1 in phase 2a trial) and GSK1070806 (IL-18 mAb in phase 1b trial) suggest novel mechanisms for refractory AD.17
Following the rapid top-line review of the promising data on new molecules, Golant concluded: "This therapeutic revolution in AD is allowing us to aim for deeper, more meaningful levels of disease control. When we see a patient we feel isn't quite hitting the mark, act on that. Let's not just look at EASI-75, let's look for EASI-90, the clearest skin, an itch-free state. We should continue to push for optimal patient outcomes by integrating the latest therapies and staying updated on emerging science."
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.