HIV and Hypertension: Notes for Primary Care
Hypertension in persons with HIV is a significant CV risk factor and should be a target of focused prevention in primary care.
Before the availability of antiretroviral therapy (ART), opportunistic infections were the greatest cause of HIV-related mortality. Thankfully, those days are behind us. Globally, there are 37 million individuals infected with HIV. Sixteen million of them are on ART. And you see many of them on a regular basis in your primary care practice.
Between 2005 and 2016 ART drug cocktails halved the mortality rate among the HIV-infected population, but over the same interval, cardiovascular (CV) mortality more than doubled in this cohort.
A
HTN in HIV-on-ART
Hypertension is more prevalent among persons with HIV-on-ART than in the general population (35% vs 30%); in persons with HIV-on-ART aged <50 years, hypertension prevalence is approximately 50%. The risk of CV events and all-cause mortality is higher in HIV-infected adults with hypertension than in adults without HIV infection who have hypertension and in those with HIV infection and normal blood pressure. A large cohort study of American veterans found a 2-fold higher risk of myocardial infarction in HIV-infected persons with hypertension vs persons with hypertension not infected with HIV.
A large cohort study of American veterans found a 2-fold higher risk of myocardial infarction in HIV-infected persons with hypertension vs persons with hypertension not infected with HIV.
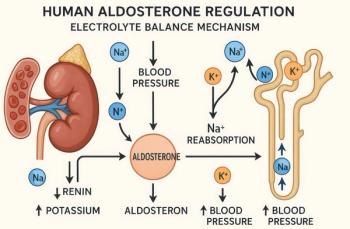
Now the logical question: what might be responsible for the rising incidence of hypertension and CVD in the HIV population? Possibilities abound, but research in this area is in its infancy. It appears that chronic inflammation as well as the impact of inflammation on the renin-angiotensin-aldosterone system (RAAS) are among the likely culprits. Hypertension in the HIV population, however, is most likely the result of a combination of factors – traditional risk factors, HIV-specific factors, and factors related to ART.
A few examples
Microbial translocation from the gut is one proposed pathophysiologic mechanism underlying hypertension in HIV-infected adults. HIV infects specific cells in the gut-associated lymphoid tissue, disrupting mucosal defense and allowing microbes to pass into the general circulation. Inflammation both in and outside the gut is one result.
Protease inhibitors (PIs), a primary component of ART regimens, accelerate inflammation as well. PIs also increase arterial stiffness, disrupt endothelial function, and are associated with lipodystrophy and dyslipidemia. In short, ART can also be a double-edged sword. PI combinations such as ritonavir/lopinavir and ritonavir/atazanavir that act on adipocytes directly activate the adipose RAAS. In one study, exposure to both combinations led to a significant increase in adipocyte angiotensin receptor protein expression after just 5 days of treatment. ART regimens are responsible for other more traditional CV risk factors, too, like lipodystrophy with central adiposity and peripheral lipoatrophy.
Acting in concert, these alterations lead to RAAS activation, with multiple consequences. HIV-infected patients have high plasma renin activity even on a low salt diet. This could be due in part to the structure of the HIV-1 protease which itself resembles renin. Leptin is increased in these individuals and it is also a RAAS activator.
Primary care physicians will continue to see larger numbers of patients with HIV controlled by ART and must be aware of their impressive cardiovascular risk profile. Unfortunately, specific research into their treatment is sparse. Small studies suggest that telmisartan, an angiotensin-receptor blocker, may combat the unique pathology in this group. Hopefully, there will be a lot more information to follow.
Reference: Fahme S, Bloomfield GS, Peck R.
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.