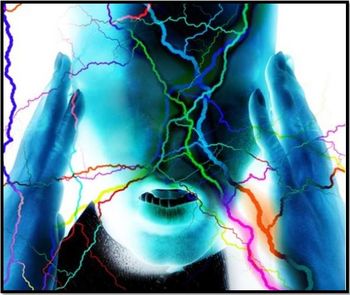
Chronic Migraines, Kids, and Cognitive Behavioral Therapy
How to treat a pediatric problem that can easily turn into a lifelong issue?
We are well aware that migraines occur in children. These tend to be shorter than in adults and treatment with analgesics tends to be successful. Unfortunately, children can develop frequent migraines-and even a chronic migraine syndrome-just like adults.
Options are limited when it comes to preventative treatment of migraine in children. Medications have been “borrowed” from adults and, when studied in children, trials have tended to be small, short, or open labeled. Except for flunarizine, which is unavailable in the US, and topiramate, which has been adequately studied in adolescents but not in younger children, all other preventative medications currently used in pediatric migraine are based on this “weaker” data or on expert opinion.1
In 2013,
If I had a “new medication” that-if combined with an older “safe” medication-could reduce migraines in up to 90% of patients by 50% or more, wouldn’t you clamor to find out about it and use it in your patients?
There were 2 major types of barriers:
. Those related to the provider/medical system (eg, the provider lacking specific knowledge of CBT, lack of time to explain CBT, and even lack of referral options)
. Those related to the patient/parents (eg, the stigma associated with mental health problems, lack of family time and interest or financial factors)
The authors explain what CBT is and even provide some samples. They offer brief, key ideas to help clinicians understand the rationale for its use that can in turn be used to explain this treatment modality to a patient and his parents. And they provide multiple ideas on how to identify local child mental health providers that can serve as a referral base and ideas on how to build up a local base of expertise that can serve some of these needs.
Finally, the authors discuss ways to overcome barriers related to the patient/their parents-from education of the patient and family on what this CBT entails to provider involvement in helping clear insurance hurdles.
Their article provides some very clear ideas on how we can be more effective in treating a pediatric problem that can easily turn into a lifelong issue.
References:
1. Lewis D, Ashwal S, Hershey A, et al, Practice Parameter: Pharmacological treatment of migraine headache in children and adolescents.
2. Powers SW, Kashikar-Zuck S, Allen J, et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents.
3. Ernst MM, O’Brien HL, Powers SW. Cognitive-behavioral therapy: how medical providers can increase patient and family openness and access to evidence-based multimodal therapy for pediatric migraine.
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.