CGRP: Taking Aim at the New Migraine Target
Promising new research is testing monoclonal antibodies delivered via infusion against CGRP, a powerful mediator of inflammation.
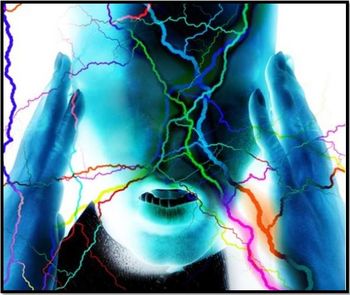
[[{"type":"media","view_mode":"media_crop","fid":"42370","attributes":{"alt":"","class":"media-image media-image-right","id":"media_crop_7005371777017","media_crop_h":"0","media_crop_image_style":"-1","media_crop_instance":"4571","media_crop_rotate":"0","media_crop_scale_h":"0","media_crop_scale_w":"0","media_crop_w":"0","media_crop_x":"0","media_crop_y":"0","style":"height: 265px; width: 265px; float: right;","title":"©art4all/Shutterstock.com ","typeof":"foaf:Image"}}]]Theories behind the mechanism of migraine headache have expanded over decades of research that has implicated various brain structures, systems, and molecules and spawned a range of antidotes. The neurotransmitter serotonin has long been viewed as a critical component in the mechanism of migraine1 and the advent of the migraine-specific abortive triptan medications revolutionized migraine treatment. As research continues, however, a serotonergic mechanism alone has come to seem insufficient as an explanation for migraines as more than one-third of patients with an acute migraine do not respond to the triptans. Other neurotransmitters, (eg neurokinin A, substance P) have been implicated in the mechanism of migraines but thus far not enough is known about their specific roles for them to become therapeutic targets.
That is, with one exception: calcitonin gene-related peptide (CGRP).2
In the 1990’s CGRP was found to trigger intense vascular dilation and inflammation in the cerebral circulation. Research into the function of CGRP has advanced to the point where some headache researchers opine that it may be the actual mediator for migraine pain and that naturally occurring serotonin in the circulation acts to block the release of CGRP and the ensuing inflammation.
This information has moved CGRP to the forefront as a therapeutic target in migraines. Neurochemists are in search of CGRP antagonists. There has been some limited success with the antagonist olcegepant delivered intravenously and some of its derivatives produced for oral ingestion. Unfortunately, hepatotoxicity from these oral CGRP antagonist formulations has slowed significantly any further advances in developing effective oral agents in this class. Intravenous therapy against CGRP is a different story.
Intravenous therapy with monoclonal antibodies (mAbs) is already an essential tool used by our colleagues in oncology, rheumatology, and more recently, neuroimmunology and it is coming to headache medicine in the near future. Several therapeutic mAbs for migraine prevention have completed phase 2 clinical trials and phase 3 trials are in progress for migraine prophylaxis and cluster headache.3 These intravenous treatments consist of arrays of mAbs that are targeted to prevent or stop the inflammation triggered by CGRP. I was reminded of the advantages, including safety and efficacy, of antibody infusion while thinking about how the use of similar smaller oral components is limited by hepatotoxicity when they are metabolized. Dr Herbert Markley, in a recent editorial in the journal Headache,4 refreshed my memory: antibody mixtures that are infused are “metabolized” not by the kidneys or liver but by the reticulo-endothelial system, a fully different pathway that bypasses physiologic limitations. In addition, the relatively long half-life of mAbs (up to several weeks) lengthens dosing intervals which can make therapy more convenient and improve patient compliance.3
Future therapy for migraineurs may look more like the treatments currently prescribed for patients with multiple sclerosis. These may range from self-administered subcutaneous or intramuscular injections to routine infusions given at infusion centers to prevent migraine headache. Targeting CRGP is only the beginning.
References:
1. Humphrey PPA, Feniuk W, Peren MJ, Beresford IJM, Kingle MS.
2. Ho T, Edvinsson L, Goadsby PJ.
3. Silberstein S, Lenz R, Xu C.
4. Markley HG.
Additional reading
Goadsby PJ.
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.