BP Control Better in Primary Care
More patients were found to be at blood pressure goal in primary care settings vs specialty practice in a new study. Our author looks at possible reasons why.
Primary care is a demanding way of life. Responsibilities keep increasing, hours get added to an already expanded day, and much like Rodney Dangerfield, the average primary care physician (PCP) doesn’t get much respect. The article that caught my attention this month is a reminder that the work of primary care is important and is achieving important goals in critical areas where specialty colleagues may not be keeping pace.
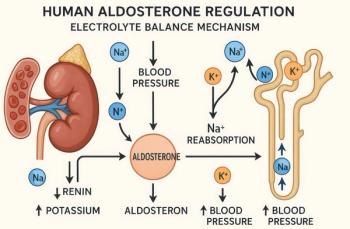
It is well-known that the cornerstone of cardiovascular risk factor management is strict blood pressure (BP) control. Although the average patient visit occurs in decreasing “snippets” of time, BP measurement is a prominent part of that visit, whether in a specialty or primary care setting. Billups and coauthors looked at BP control in primary care and specialty practices in the UCHealth Integrated Network, an accountable care organization in the Denver metropolitan area. The records of >86 000 patient visits for the year 2016 were studied.
The results are interesting.
Those patients whose most recent BP measurement was performed in a specialist office (n=43 364) were significantly less likely to be at goal vs those (n=43 148) whose most recent measurement was in primary care (63% vs 68%, respectively, OR = 0.83 [0.80â0.85]). A total of 27 955 patients had blood pressure measurements performed in both settings over the year and the control rates of BP based upon the most recent specialty and primary care measurements were 63% and 71%, respectively (OR = 0.62, 0.60-0.65).
Control was appreciated more often in the primary care setting.
If the specialty-primary care BP measures were compared on visits that were within 7 days of each other, the difference persisted, leading one to suspect that the measurement of blood pressure in 1 of the 2 settings may have not been accurate. Do all medical settings follow carefully the 2017 American Heart Association
This paper piqued my interest for more than one reason. First, kudos to those many PCPs who labor long and do not receive enough praise for a job well done. But on another level, assuming that the better control of blood pressure achieved in primary care vs specialty practice may be a byproduct of optimal and consistent technique, the issue of blood pressure management just became a lot more complicated.
Source: Billups SJ, Saseen JJ, Vande Griend JP, Schilling LM.
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.