Atopic Dermatitis Update: Roflumilast 0.15% Cream Shows Long-Term Safety and Efficacy Plus Benefit with Proactive Use
Improvement in AD signs and symptoms continued through 56 weeks of treatment with the PDE4 inhibitor including when used just twice weekly as prophylaxis.
The study also showed that roflumilast application twice weekly by individuals who had achieved clinical clearance after 4 weeks of daily use maintained improvement in AD signs and symptoms for more than 200 days, "demonstrating the efficacy of proactive treatment as an alternative to reactive treatment for improved long-term outcomes," study authors wrote in the journal Dermatitis.
The 52-week, phase 3, OLE trial enrolled 658 patients aged 6 years and older who had completed a previous 4-week phase 3 clinical trial with roflumilast, ie, were rolled over from the pivotal phase 3 studies INTEGUMENT-1 and INTEGUMENT-2. Participants applied roflumilast 0.15% once daily for the initial 4-week treatment period after which those who had achieved a Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) score of 0 (clear) switched to proactive twice weekly roflumilast application to normal appearing but flare-prone areas.
To evaluate the long-term safety of once-daily application, first author Eric L Simpson MD, MCR, Frances J. Storrs Medical Dermatology Professor at Oregon Health & Science University, and colleagues, evaluated adverse events (AEs), investigator- and patient-rated local tolerability assessments, vital signs, and clinical laboratory parameters. Efficacy endpoints included the proportion of participants who achieved vIGA-AD 0/1 (clear/almost clear), Worst Itch-Numeric Rating Scale (WI-NRS) success (defined as a 4 point or greater reduction), and 75% or greater improvement in Eczema Area and Severity Index (EASI-75).
Of participants in the 24-week cohort, 75.9% completed the trial; 57.7% of those in the 52-week cohort were completers, according to the study. Mean age was 19.4 years in the roflumilast group and 20.5 years in the vehicle group; approximately 40% were aged 6 to 11 years and 33% aged 12 to 17 years. Women comprised approximately 56% of both groups.
Approximately three-quarters of study participants had moderate disease. At trial baseline, 26.2% of participants treated with roflumilast had vIGA-AD of Mild and 73.8% had vIGA-AD of Moderate. Of participants treated with vehicle, 26.0% had vIGA-AD of Mild and 74.0% had vIGA-AD of Moderate.
FINDINGS
Researchers reported a mean EASI score of 10.39 for roflumilast-treated participants and 10.58 for the vehicle group at the outset of the parent trial. They recorded a mean BSA involvement of 14.4% in the roflumilast group and 12.9%in the vehicle group.
Safety outcomes. Simpson and colleagues documented treatment-emergent adverse events (TEAEs) in 241 participants (36.7%), with most reported as mild or moderate in severity. The research team reported TEAEs it considered related to the study treatment in 31 (4.7%). Serious AEs were reported in 8 (1.2%) participants, though none were judged to be treatment related. The most common TEAEs were COVID-19 (4.6%), upper respiratory tract infection (3.2%), nasopharyngitis (3.0%), and headache (2.7%). Less than 1% (0.5%) of participants reported mild or moderate application site pain. The researchers reported no significant effects of roflumilast 0.15% on vital signs, clinical laboratory results, depression, or suicidal ideation.
Efficacy outcomes. Improvement in treatment efficacy was observed throughout the parent trial, according to the results, with 56.6% of participants treated with roflumilast continuously and 53.8% of patients who switched from vehicle to roflumilast achieving vIGA-AD 0/1 at week 56.
Two-thirds (66.2%) of participants achieved EASI-75 in the roflumilast group as did a comparable proportion (64.6%) in the vehicle group. Similar proportions of both groups also achieved WI-NRS success (56.9% in the roflumilast group, 50.0% in the vehicle group) while WI-NRS 0/1 (no or minimal itch) was reached by 45.9% and 50.0% of the participants, respectively.
Of the 130 participants who switched to proactive biweekly dosing after achieving vIGA-AD 0, 57.7% maintained disease control through the final study visit, with a median duration of 281 days.
Among the study’s limitations, Simpson et al note failure to assess participants’ palms and soles and omission of the scalp for treatment or evaluation. They also suggest that additional research on younger populations is needed.
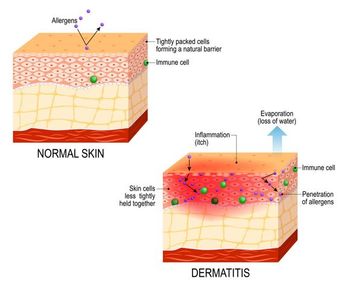
Flares are a universal part of the course of AD and typically understood to be disease worsening requiring escalation or intensification.2 Flare prevention and minimizing the frequency and severity of the episodes are central to establishing long-term disease control, according to experts.2
The research team concludes that when used proactively, roflumilast cream could reduce the need for reactive treatment of flares, which often requires use of topical or systemic corticosteroids. Further, the authors cite evidence that “proactive treatment has the potential to reduce the chronicity of AD by addressing the elevated levels of inflammatory mediators that remain in previously active areas of AD, even after clearance.”
1. Simpson EL, Eichenfield LF, Papp KA, et al. Long-term safety and efficacy with roflumilast cream 0.15% in patients aged ≥6 years with atopic dermatitis: a phase 3 open-label extension trial. Dermatitis. Published online January 10, 2025. doi:10.1089/derm.2024.0418
2. Girolomoni G, Busà VM. Flare management in atopic dermatitis: from definition to treatment. Ther Adv Chronic Dis. 2022;13:20406223211066728. doi: 10.1177/20406223211066728
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.