
How many cases of COVID-19 have been confirmed globally and nationally? How many recoveries? Get your daily COVID-19 update here.

How many cases of COVID-19 have been confirmed globally and nationally? How many recoveries? Get your daily COVID-19 update here.
A NIH clinical trial begins today that will compare antiviral remdesivir alone to remdesivir plus anti-inflammatory baricitinib in patients critically ill with COVID-19.

Authors of a new study found no association between treatment with high blood pressure drugs and an increased risk of contracting novel COVID-19.

Americans are stocking up on prescriptions, wearing masks when they go out, are afraid for their mental health, and some will refuse a COVID-19 vaccine.

Get the latest data on confirmed cases, recoveries, and more with our daily COVID-19 update.
Anticoagulation was associated with increased survival time and bleeding events were similar between treated and non-treated patients.

Get the latest data on confirmed cases, recoveries, and more with our daily COVID-19 update.

Researchers recently launched CHASING COVID, the only national cohort study focused on the COVID-19 pandemic.

The FDA issued an emergency use authorization to Gilead Sciences, Inc, for remdesivir for the treatment of suspected or laboratory-confirmed COVID-19.

Medicare and Medicaid will now cover many more services provided via telehealth, particularly by audio-only telephone.

Get the latest data on confirmed cases, recoveries, and more with our daily COVID-19 update.
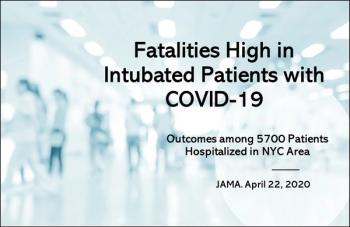
Study: Nearly 90% of inpatients with COVID-19 on mechanical ventilation died; obesity, diabetes, hypertension common among the 5700 patients.

Results of the phase 3 INTERCEPT trial showed that patients who received treatment with novel AXS-07 had substantially reduced migraine pain.

Primary care physicians can recommend a growing range of programs, online and off, designed to help patients lose weight in a healthy way, with support.

To start, it requires appreciation of the sensitive nature of discussions around obesity and weight loss, says well-known obesity expert Donna H. Ryan, MD.

The first diagnostic test with a home collection option for COVID-19 was recently authorized by the FDA.
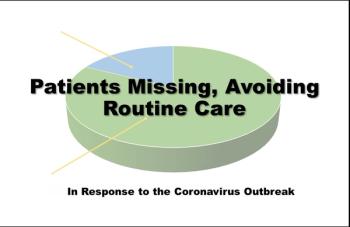
More than 10% of survey repondents with chronic illness (eg, asthma, diabetes), would avoid seeking needed care because of fears related to COVID-19.

Get the latest data on confirmed cases, recoveries, and more with our daily COVID-19 update.

Get the latest data on confirmed cases, recoveries, and more with our daily COVID-19 update.

There is no pharmacologic agent proven to be safe and effective for treating COVID-19, according to guidelines compiled by an NIH-assembled panel of experts.