
The 2% preparation of an allylamine antifungal is a new addition to the menu of available topical agents. It has the advantage of once-daily dosing and shorter course of therapy.

The 2% preparation of an allylamine antifungal is a new addition to the menu of available topical agents. It has the advantage of once-daily dosing and shorter course of therapy.

A 57-year-old man presented for medical evaluation because of the presence of a "funny looking lump" on the lateral aspect of his right upper thigh.
An 88-year-old woman sought medical attention for a nodule on the anterior surface of her left foreleg that had gradually developed.

This large bruise developed after the patient had an accident in her yard. Post-traumatic subcutaneous hematomas are common in elderly women, especially those who are anticoagulated. Untreated, the hematoma can eventuate into an abscess and even sepsis.

This lesion looks like basal cell or squamous cell carcinoma, but biopsy showed it to be an idiopathic inflammatory disorder of the external ear. Skin cancers of the pinna are rarely painful, as this lesion was.

This uncommon benign entity closely mimics squamous cell carcinoma, superficial basal cell carcinoma, and advanced actinic keratoses. The lichenoid keratosis does not transform into skin cancer.

The only impressive thing about this lesion was a “notch” in its superior pole, and some mild pigment heterogeneity. Prudent caution proved extremely beneficial. The history of a “new” lesion in a patient with almost no visible nevi, along with some very subtle gross features, led to early recognition and elimination of a malignant melanoma.

It is often surprising how wide and how deep skin cancers have already spread, despite a relatively small-looking superficial component. This patient had a history of melanoma in situ.

The first appropriate use criteria for any test or treatment within the field of dermatology were developed recently.

Consider all relevant factors when deciding what steps to take with a pigmented lesion noticed by the patient or encountered during a routine physical examination.

Almost no benign disorder affecting nasal skin should bleed.

Always check the toenails for fungal infection after diagnosing tinea pedis, corporis, or cruris. The toenails may act as the source of infection and a reservoir, which may lead to reinfection after the cutaneous dermatophytosis is cleared.

The eccentric placement of a darker spot within the overall lesion should raise suspicion for melanoma. This lesion’s asymmetry is the most worrisome feature. The need for histologic examination is clear in such cases.

The lesion’s location, along with visible telangiectasia on the lesion’s surface, suggest a basal cell carcinoma.

Note that some lesions occur within the outer ear, quite typical for the diagnosis of discoid lupus.

Up to 80% of those with necrobiosis lipoidica have diabetes mellitus; however, this disorder develops in fewer than 1% of people who have diabetes.

Elevated serum uric acid level is pathognomonic for gout. Untreated gout may lead to tophi, nephropathy, and uric acid nephrolithiasis.

This solitary, fairly well-defined whitish plaque, surrounded by a broad band of violaceous erythema is a classic presentation of the “lilac ring” phase of early morphea. Potent corticosteroids led to prompt resolution.

The differential diagnosis includes figurate erythema, granuloma annulare, sarcoidosis, and Hansen’s disease. Additional history disclosed that the plaques expanded, migrated and disappeared over a matter of days, eliminating all but the correct diagnosis: figurate erythema, a reactional (hypersensitivity) state.

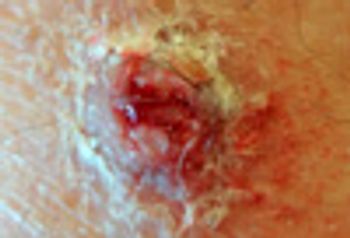
The location (pretibial surface) of this ulcer, its visibly rolled undermined border, and severe pain are all typical of pyoderma gangrenosum, which is typically associated with inflammatory bowel disease, rheumatoid arthritis, and hematologic malignancies.

This is the most common form of amyloid deposition in the skin. It is not associated with the systemic disease, but is solely a cutaneous malady.

Syphilis is often called the "great imitator." The slides that follow show syphilis in various guises-and various disorders that can mimic the cutaneous manifestations of the sexually transmitted infection.

The shiny white and atrophic skin involving the vulva and perirectal skin is nearly pathognomonic for lichen sclerosus et atrophicus This inflammatory disorder of unknown etiology gradually increases in intensity.

Erythema multiforme; Rocky Mountain Spotted Fever; syphilis; pityriasis rosea. . . which of these disorders is the most likely cause of these macular lesions?

These whitish colored lesions were the result of lichen planus. Hepatitis C virus infection should be sought, since this viral infection is often associated with recent-onset lichen planus in younger persons.